Effect of maternal age on cord blood nutrients and birth weight at term
I. Onyesom1 , A.E. Oshunloye1 , U.E. Uzuegbu1 and S.M. Suru2 *
1
Department of Medical Biochemistry,
Delta State University,
Abraka
2
Nutritional Biochemistry Unit, Department of Biochemistry,
University of Ibadan,
Ibadan
DOI: http://dx.doi.org/10.12944/CWE.3.1.04
Adequate nutrition has been reported to increase the frame size and birth weight of neonates at term. These anthropometric measures have been used to predict foetal growth and well-being. It has been observed that the amounts of maternal serum and cord blood glucose influence these anthropometric parameters. Therefore, this study reports the relationship between maternal age and some biochemical indices of foetal nutrition (maternal serum and cord blood glucose, and birth weight at term). Pregnant subjects between 15 and 45 years, and who were about to be delivered were selected from the Labour room, Central Hospital, Warri, Delta State, Nigeria. Cases of complications and disease conditions were excluded. Weight and age-matched, non-pregnant women in apparent good health were randomly recruited as control subjects. The results show that younger (15-19years) and older (40-45years) pregnant women had reduced blood glucose (4.42±1.31mmol/L: R>0.05 and 3.52±1.49mmol/L: R>0.05) levels, and this consequently, reduced babies cord blood glucose (3.28±0.98mmol/L:R<0.05 and 2.81±0.79mmol//L:R<0.05) and birth weight (3.28±0.77kg and 3.10±0.63kg) at term. Maternal serum glucose of the pregnant women between 20-39 years was 4.65±1.39mmol/L. The cord blood glucose and birth weight of their neonates at tem were 3.51±1.16mmol/L and 3.48±0.70kg. Special prenatal care should be given to these categories of pregnant women (15-19 and 40-45years) in Nigeria, in order to minimize or if possible, eliminate the medical complications associated with small foetal size and low birth weight.
Copy the following to cite this article:
vol3no1/CWEVO3NO1P27-30.pdf Onyesom I, Oshunloye A.E, Uzuegbu U.E, Suru S.M. Effect of maternal age on cord blood nutrients and birth weight at term. Curr World Environ 2008;3(1):27-30 DOI:http://dx.doi.org/10.12944/CWE.3.1.04
Copy the following to cite this URL:
Onyesom I, Oshunloye A.E, Uzuegbu U.E, Suru S.M. Effect of maternal age on cord blood nutrients and birth weight at term. Curr World Environ 2008;3(1):27-30. Available from: http://www.cwejournal.org/?p=734
Download article (pdf)
Citation Manager
Publish History
Select type of program for download
| Endnote EndNote format (Mac & Win) | |
| Reference Manager Ris format (Win only) | |
| Procite Ris format (Win only) | |
| Medlars Format | |
| RefWorks Format RefWorks format (Mac & Win) | |
| BibTex Format BibTex format (Mac & Win) |
Article Publishing History
| Received: | 2008-03-18 |
|---|---|
| Accepted: | 2008-05-06 |
Introduction
Pregnancy is a complex nutritional exercise that involves the arrangement and transport of nutrient materials for foetal metabolism and the provision of good internal environmental conditions suitable for foetal growth. One of the basic nutrients required for foetal nourishment is glucose, and the control of glucose intake by pregnant women has been reported to influence birth weight.¹
Transplacental glucose transport is a facilitated process and in humans, it is mediated by the glucose transporter isoform, GLUT 1 which is highly abundant in the syncytiotrophoblast plasma membrane. Therefore, net transport is highly dependent on maternal blood levels². GLUT 1 glucose-transporting capacity might be as much as 20 fold higher than basal membrane transport capacity, which is rate limiting, hence any alteration in basal membrane transport of glucose would affect net transport across the placenta. The number of GLUT 1 transporter per membrane area in basal membrane vesicles increases during the first half of the gestational period and remains constant thereafter, suggesting that early pregnancy is a critical period in establishing the glucose-transporting capacity of the human placenta.2,3 High glucose concentrations down-regulate GLUT 1 expression in a variety of cell culture systems but in placenta cells, pronounced hyperglycaemia appears to be required to alter GLUT 1 expression and activity.4,5 Placental glucose transporters are sensitive to regulation by nutrient availability mainly during early pregnancy.6
Perinatal and neonatal mortality rate is a function of birth weight and this decreases with increasing birth weight, though to a limit of about 4.0kg, after which mortality rate increases.7 Thus, low birth weight infants have been shown to be at much higher risk of perinatal death and growth difficulties,7 and the identified risk factors include: ethnicity, genetic, lower socioeconomic status, lower pregnant weight, smaller pregnancy weight gain, alcohol consumption, maternal smoking during pregnancy, maternal hypertension, infection during pregnancy, perceived psychologic stress, prior adverse pregnancy outcome and multiple births.8 Therefore, prevention of low birth weight should be an important health goal.
Gravid (gestational) diabetes results to increased birth weight which could induce cesarean delivery and other birth trauma.9 Similar complications include, birth injuries, intellectual and developmental retardation.10 The impact of gestational diabetes on the foetus depends on maternal derangements in glucose metabolism and alterations in placental transport characteristics.1
This present study attempts to report the influence of maternal age on neonatal birth weight, and maternal and cord blood glucose-the main source of energy during pregnancy, and the primary determinant of foetal nutritional status.
Material and Methods
Subjects
The subjects were selected at random from the Labour Unit, Central Hospital, Warri, Delta State, Nigeria, and these include pregnant women who were about to be delivered. Their ages were between 15 and 45 years. All cases of complications and disease conditions associated with pregnancy were excluded in the study. Weight and age-matched, non-pregnant women in good health were recruited as control subjects for the study.
Specimen Collection and Analysis
The normal process of vein puncture technique using needle and syringe was used to collect blood samples from the participants. Cord blood specimens were also collected from the neonates by introducing the needle into the umbilical vein at any point on the umbilical cord.
The blood sample collected into fluoride oxalate bottle was centrifuged within 30 min of collection at 1200 × g for 5 min at room temperature to get about 1.0ml of plasma. The plasma samples were stored frozen in bijou bottles, and analysed for glucose within 48h.
The glucose levels of the plasma specimens were determined by the glucose oxidase method¹¹ using commercially prepared reagent kit (Randox Laboratories, Ardmore, UK).
The birth weights of the neonates were taken and recorded to the nearest 0.1kg.
Statistics
All statistical calculations were performed by the SPSS-PC programme package (version 7.5).
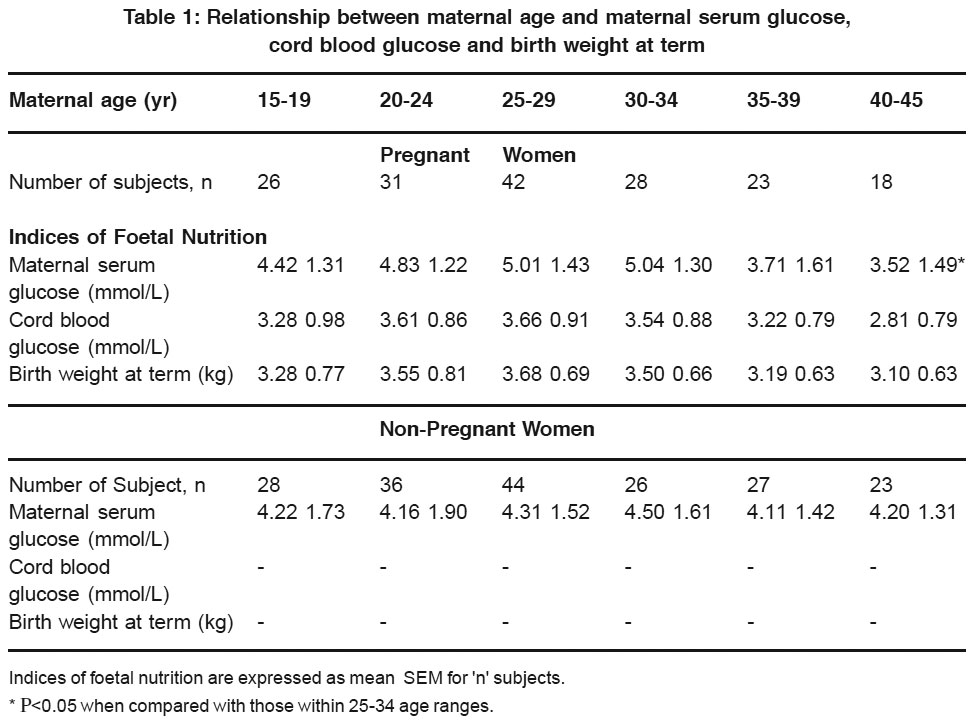 |
Table 1: Relationship between maternal age and maternal serum glucose, cord blood glucose and birth weight at term Click here to view table |
Results
The results obtained show that there was no demonstrated significant difference (R>0.05) in glucose levels between the pregnant and non-pregnant women in all the age brackets studied. On the average, however, the blood glucose levels for the pregnant women at term were observed to be higher (except for 35-39 and 40-45 age ranges) peaking at 25-29 age range (Table 1).
Older pregnant women above 35 years, and young ladies below 20 years had reduced blood glucose levels when compared with those between 20-24, 25-29 and 30-34 years. The difference between those within 20-34 years, “the child bearing age” and those above 35 years was statistically significant (Ρ<0.05).
The influence of maternal age on the cord blood glucose seems similar, though maternal serum glucose level was calculated to be 34.8%, 33.8%, 36.9%, 42.4%, 15.2% and-9.4% different from the cord blood level at the various age categories, respectively. These differences were not significant (Ρ>0.05). Maternal age affects both maternal and cord blood glucose levels.
The amount of glucose in the umbilical cord blood could determine foetal weight, and in apparent good health, this appears to be dependent on the maternal level and age.
Discussion
Pregnant women between the ages of 15 and 34 years have higher levels of glucose at term when compared with the non-pregnant women at the different maternal ages, though not statistically significant (Ρ>0.05). This agrees with the observation of Yen (12) who reported an increase in maternal blood glucose during the child bearing ages (18-35 years). Pregnancy-induced increase in blood glucose is due to hormonal action which causes increased gluconeogenesis and protein metabolism to meet the glucose (energy) demand caused by the physiochemical changes associated with pregnancy and this prepares nutrient materials for foetal metabolism, growth and development. Nevertheless, it was observed that pregnant women above 35 years had demonstrated decrease in the level of plasma glucose. It therefore, appears that maternal age affects blood glucose. This could imply that preparation and mobilization of basic nutrients, to be transported for foetal health may be inadequate since the foetus does not synthesize its own nutrient but depends on maternal source.
The effect of maternal age on cord blood glucose was observed to be same, and so the changes in maternal blood glucose, correlates positively with cord blood glucose (r = 0.452; P<0.05). Udo, et al13 have reported similar relationship between maternal and cord blood glucose. It follows that maternal nutritional state could modulate foetal nutrient status.
From this study, it was observed that both maternal and cord blood glucose strongly influence neonatal birth weight positively. Previously, Coustan and Imarah,9 and Adams, et al14 have observed increased neonatal birth weight in women with higher maternal blood glucose.
Evidence from this present study suggests that maternal age could affect the arrangement and transport of glucose for foetal well-being. Older women above the age of 35 years, and who have had multiple births especially, demonstrated reduced blood glucose and consequently, gave birth to infants with lower birth weigh. This could be worrisome since low birth weight infants have been reported to be at much higher risk of perinatal death and growth difficulties.7 It is therefore, recommended that among the Nigerian pregnant population, women above 35 years, who have had multiple births especially, and younger women below 20 years should be specially monitored to avoid giving birth to babies with small body size and low weight at term.
Acknowledgements
The authors wish to appreciate the management of Central Hospital, Warri, for their co-operation, and specially thank the staff members of the Chemical Pathology Laboratory Unit for their technical assistance.
References
- Jansson, T., Wenergren, M, and Powell, T.L.: Placental glucose transport and GLUT 1 expression in insulin-dependent diabetes. Am. J. Obstet. Gynecol. (1999) 180: 163-168.
- Jansson, T., Wannergren, M. and Illsley, N.P.: Glucose transporter protein expression in human placenta throughout gestation and in intrauterine growth retardation J. Clin. Endocrinol, Metab. (1993) 77: 1554-1562.
- Hahn, T. and Desoye, G.: Ontogeny of glucose transport systems in the placenta and its progenitor tissue. Early Preg. (1996) 2: 168-182.
- Illsley, N.P.: Expression of the human placental glucose transporter is not subject to significant regulation by glucose concentration. Soc. Gynecol. Invest. (1995) 2: 285-289.
- Meuckley, M.: Facilitive glucose transporters. Eur. J. Biochem. (1994) 219: 713-725.
- Jansson, T., Extrans, Y., Wennergren, M. and Powell, T.L.: Placental glucose transport in gestational diabetes mellitus. Am. J. Obstet. Gynecol. (2001) 184: 111-116.
- Campbell, M.K. and Mottola, F.M.: Recreational exercise and occupational activity during pregnancy and birth weight: A case-control study. Am J. Obstet. Gynecol. (2001) 184 (3): 403-408.
- Campbell, M.K., Halinda, E., Carlyle, M.J., Fox, A.M., Turner, L.A. and Chance, G.W.: Factors associated with follow-up clinic attendance and developmental outcome in infants of low birth weight. Am. J. Epidemiol. (1993) 138: 704-713.
- Coustan, D.R. and Imarah, J.: Prophylactic insulin treatment of gestational diabetes reduces the incidence of macrosomia operative delivery and birth trauma. Am. J. Obstet. Gynecol. (1984) 150: 836-842.
- Babson, S.G., Behrman, R.E. and Lesel, R.: Fetal growth; live born birth weight for gestational age of White middle class infants. Pediatrics. (1970) 45: 237-347.
- Barham, D. and Trinder, P., Quantitative determination of glucose using GOD-PAP method. Analyst, (1972) 97: 142-146.
- Yen, S.S.: Endocrine regulation of metabolic homeostasis during pregnancy. Clin. Obstet. Gynecol. (1993) 16: 130-137.
- Udo, A.E., Udousoro, N. and Archibong, E.T.: Evidence of glucose gradient along the umbilical cord: implication for fetal development. AMLSN Bronchure for the 20th Annual Scientific Conference, Calabar. (1996) 9-10.
- Adams, K.M., Li, H., Nelson, R.L. Ogburn, P.L. and Danilenko-Dixon, D. R.: Sequelae of unrecognized gestational diabetes. Am. J. Obstet. Gynecol. (1998) 178: 1321-1332.






