AHP and GIS-based Risk Zonation of COVID-19 in North East India
Corresponding author Email: ranjit.mahato@rgu.ac.in
DOI: http://dx.doi.org/10.12944/CWE.15.3.29
Copy the following to cite this article:
Mahato R, Bushi D, Nimasow G. AHP and GIS-based Risk Zonation of COVID-19 in North East India. Curr World Environ 2020;15(3). DOI:http://dx.doi.org/10.12944/CWE.15.3.29
Copy the following to cite this URL:
Mahato R, Bushi D, Nimasow G. AHP and GIS-based Risk Zonation of COVID-19 in North East India. Curr World Environ 2020;15(3). Available From: https://bit.ly/3gb6EA6
Download article (pdf)
Citation Manager
Publish History
Select type of program for download
| Endnote EndNote format (Mac & Win) | |
| Reference Manager Ris format (Win only) | |
| Procite Ris format (Win only) | |
| Medlars Format | |
| RefWorks Format RefWorks format (Mac & Win) | |
| BibTex Format BibTex format (Mac & Win) |
Article Publishing History
| Received: | 17-06-2020 |
|---|---|
| Accepted: | 17-11-2020 |
| Reviewed by: | 
 Gadekar Janardhan
Gadekar Janardhan
|
| Second Review by: |

 Paul Thaddeus Kazibudzki
Paul Thaddeus Kazibudzki
|
| Final Approval by: | Dr. Mohammad Oves |
Introduction
The World Health Organization (WHO) country office has been informed about the pneumonia cases of unknown etiology detected in Wuhan City, Hubei Province of China on 31st December 20191. Unexpectedly, it spread to different regions of China as well as other countries across the world, despite China’s considerable efforts to restrain the infection within Hubei2. Later, the epidemic was recognized as novel coronavirus of 2019 or SARS-CoV-2 resulting in the disease COVID-193. On 31st January 2020, the WHO declared coronavirus as a public health emergency of international concern4. It is a member of a large family of coronaviruses resulting in Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS)5. Compared to the SARS-CoV (2002/2003) and the MERS-CoV (2012-2014), COVID-19 has remarkably faster human-to-human transmission as it took only 48 days to infect 1000 people, whereas MERS took around 2½ years and SARS took about four months to reach that figure2. Based on the global spread of COVID-19, the WHO declared it as a pandemic6. In general, the virus is capable of infecting people of all ages, but the population with above 60 years of age and people with heart disease, asthma, diabetes, chronic lung disease, kidney disease, etc. are at increased risk of severity of COVID-197.
Although health facilities and socio-economic conditions of the people have drastically improved since independence, human development and its growth are destitute in North East India (NEI, hereafter). In fact, it is lower than many underdeveloped nations of the world8. Since the initial detection of COVID-19 in Kerala on 30th January 2020, it had spread to many parts of the country. Presently, there are 276,583 confirmed cases, 7,745 deaths, and 135,205 cured cases of COVID-19 in the country as on 10th June 20209. The cases have increased tremendously from 519 confirmed cases with ten deaths as of 24th March 2020 to date. NEI is located in the easternmost part of the country, which is inhabited by 3.88% of the country’s total population. The earliest infection of COVID-19 in NEI was reported from Manipur on 24th March 202010, and it took only 78 days to reach 4,433 confirmed cases as of now9. The number of cases has been increasing despite the entire nation been put under lockdown (in different phases) from 25th March 2020 by the central government11. Due to the absence of a vaccine, avoidance of touching the nose, eyes, and mouth, frequently washing hand, the practice of hand sanitizers, covering of face with a proper quality mask, social distancing, and respiratory hygiene are the quotidian measures to stay safe from the virus5. The inherent large-scale regional disparities in terms of demography and socio-economic characteristics, along with depressed health conveniences, are likely to exacerbate the pandemic situation in the region. Therefore, an effort has been made to delineate the risk zones of COVID-19 in NEI using the data gathered from various sources of the Government of India applying Analytic Hierarchy Process (AHP) and Geographical Information System (GIS).
Materials and Methods
Study Area
The study area constitutes 8 NEI states, namely Arunachal Pradesh, Assam, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim, and Tripura (Fig. 1). The region is characterized by mountains, hills, and plains with rich culture and biological diversity. NEI shares an international boundary with Nepal, China, Bhutan, Myanmar, and Bangladesh and a state boundary with West Bengal.
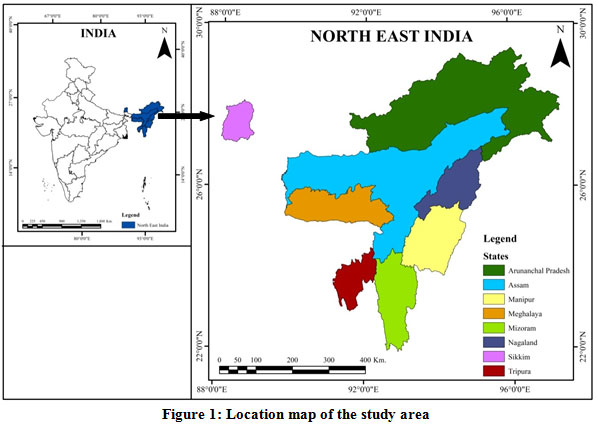 |
Figure 1: Location map of the study area Click here to view figure |
Methodology
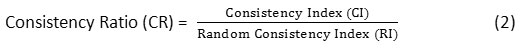
Based on promoting and controlling factors of COVID-19, fourteen thematic layers (Figures 1 & 2) have been considered to carry out the present study using ArcGIS 10.3 software. AHP was used to assign the weights for each individual reclassified layer (generated after converting ancillary data into raster format) to perform the Weighted Overlay technique to generate the final risk zonation map of the study area.
Table 1: Database and Sources
|
Sl. No. |
Thematic Layers |
Sources |
Website |
|
1. |
Population size (Projected Population, 2020) |
National Health Profile, 2019, Central Bureau of Health Intelligence, Govt. of India (GoI). |
https://www.cbhidghs.nic.in12 (Accessed on 10th April 2020) |
|
2. |
Population Density |
Calculated using projected population, 2020 and Census data. |
https://www.census2011.co.in13 (Accessed on 10th April 2020) |
|
3. |
Urban Population |
Population Projections for India and States 2011-2036, National Commission on Population, Ministry of Health & Family Welfare. |
https://nhm.gov.in14 (Accessed on 25th April 2020) |
|
4. |
Elderly Population |
Population Census 2011, after Elderly in India, 2016, Central Statistics Office, GoI. |
http://mospi.nic.in15 (Accessed on 25th April 2020) |
|
5. |
Population Below National Poverty Line |
NITI Aayog, after Progress Report, 2020, Ministry of Statistics and Programme Implementation, GoI. |
http://www.mospi.gov.in16 (Accessed on 25th April 2020) |
|
6. |
Percentage of Marginal Workers |
Basic Statistics of North Eastern Region 2015, North Eastern Council Secretariat (Evaluation and Monitoring Sector), GoI. |
http://necouncil.gov.in17 (Accessed on 15th May 2020) |
|
7. |
Availability of Doctors |
The Health Workforce in India, WHO. |
https://www.who.int18 (Accessed on 10th April 2019) |
|
8. |
Availability of Other Health Workers |
The Health Workforce in India, WHO. |
https://www.who.int18 (Accessed on 10th April 2019) |
|
9. |
Number of Public Health Facilities |
Ministry of Health and Family Welfare, GoI. |
https://pib.gov.in19 (Accessed on 30th April 2020) |
|
10. |
Bed available in Public Health Facilities |
Ministry of Health and Family Welfare, GoI. |
https://pib.gov.in19 (Accessed on 30th April 2020) |
|
11. |
Good Governance Index (Public Health Ranking) |
Department of Administrative Reforms & Public Grievances, GoI. |
https://pib.gov.in20 (Accessed on 25th April 2020) |
|
12. |
Good Governance Index (Composite Ranking) |
Department of Administrative Reforms & Public Grievances, GoI. |
https://pib.gov.in20 (Accessed on 25th April 2020) |
|
13. |
Per Capita Income of states |
Economic & Statistical Organization, Punjab and Central Statistical Organization, New Delhi |
https://www.esopb.gov.in21 (Accessed on 30th April 2020) |
|
14. |
Number of Testing Laboratories for COVID-19 (As on 11th June 2020) |
Indian Council of Medical Research, Department of Health Research, GoI. |
https://www.icmr.gov.in22 (Accessed on 11th June 2020). |
|
15. |
COVID-19 cases (As on 11th June 2020) |
Ministry of Health and Family Welfare, GoI. |
https://www.mohfw.gov.in9 (Accessed on 11th June 2020). |
Analytic Hierarchy Process (AHP)
As per the literature review of available materials and expert opinions, Saaty’s fundamental 9 - points scale values were assigned to each thematic layer according to their potentiality on generating risk zones of COVID-19. The weights assigned to different layers were normalized and checked for consistency (consistency ratio) as suggested by Saaty (1980)23. The consistency ratio reflects the probability that the matrix ratings were randomly generated. The consistency ratio was derived using the following equations:
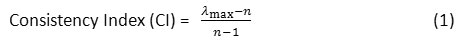
Where, is the largest eigenvalue of the pairwise comparison matrix, ‘n’ represents the total number of parameters.
is the largest eigenvalue of the pairwise comparison matrix, ‘n’ represents the total number of parameters.
The value of the Random Consistency Index (Table 2) was obtained from Saaty (1980)23. For consistent weights, the value of CR should lie between 0 and 0.1 (i.e., 10%); otherwise, the corresponding weights should be re-evaluated. In this study, the consistency ratios of pairwise comparison matrix for promoting and controlling factors were 0.044 and 0.025, indicating that the comparisons of evaluation criteria are consistent.
Table 2: Random Consistency Indices (RI) adopted from Saaty, (1980 p. 21)23.
|
N |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
|
RI |
0 |
0 |
0.58 |
0.9 |
1.12 |
1.24 |
1.32 |
1.41 |
1.45 |
1.49 |
 |
Figure 2: Methodology used for assessing the risk zonation of COVID-19 Click here to view figure |
Delineation of Risk Zones
The factors (promoting and controlling) undertaken to carry out the study are considered to have the potentiality to influence risk during any kind of pandemic situation (Annexure 1 & 2). These influencing factors are weighted as per their response to taking risk where the higher value in promoting factors represents a high potential to promote risk, and the lower value in controlling factors represent high potentiality to defeat the risk. A weighted overlay analysis was executed using both the factors (Fig. 2) in the GIS environment to delineate the risk zones using the following formula:
PF = (PNwPNr)+(PDwPDr)+(UPwUPr)+(EPwEPr)+(BPwBPr)+(MWwMWr).
CF = (DNwDNr)+(HWwHWr)+(PHwPHr)+(BDwBDr)+(GHwGHr)+(GCwGCr)+(PCwPCr)+ (TLwTLr).
RZ = (PFwPFr)+(CFwCFr).
[Where, PF: promoting factor; CF: controlling factor; RZ: risk zone; PN: population size; PD: population density; UP: urban population; EP: elderly population; BP: population below national poverty line; MW: % of the marginal worker; DN: availability of doctors; HW: other health workers; PH: public health facilities; BD: bed available in public health facilities; GH: good governance health index; GC: good governance composite index; PC: per capita income; TL: available testing laboratories].
Results and Discussion
All the sub-criteria of selected thematic layers were assigned relative ranks based on their influence in promoting and controlling the situation (Table 4 & 6). The overall potentiality of promoting and controlling the COVID-19 pandemic has been generated through overlay analysis of the layers. Finally, the risk zones were delineated out of the promoting and controlling layers by providing equal importance (Table 7).
Promoting Factors
Among the promoting factors (Annexure-1) that would increase the cases of COVID-19 in NEI, the dominant factors (Table 3) are the concentration of urban population (24.57%), followed by population density (22.18%), population below national poverty line (25.19%), population size (13.89%), percentage of marginal workers (11.09%) and percentage of the elderly population (8.70%). As the nature of the virus is human-to-human contagious, the factors that promote human gathering and make trouble to stay inside the home for a longer time get higher weights of influence. The results based on relative weights (Table 4) and overlay analysis (Fig. 4) vary from 2.70-5.56 that was categorized into five classes using Natural Breaks (Jenks) method and represented as very high (4.50-5.56), high (3.99-4.50), moderate (3.30-3.99), low (2.88-3.30) and very low (2.70-2.88).
Table 3: Pairwise comparison matrix of promoting factors
|
PN |
PD |
UP |
EP |
BP |
MW |
Normalized Weight |
In % |
|
|
PN |
1.00 |
0.50 |
0.50 |
2.00 |
0.50 |
2.00 |
0.1389 |
13.89 |
|
PD |
2.00 |
1.00 |
0.50 |
2.00 |
2.00 |
2.00 |
0.2218 |
22.18 |
|
UP |
2.00 |
2.00 |
1.00 |
2.00 |
1.00 |
2.00 |
0.2457 |
24.57 |
|
EP |
0.50 |
0.50 |
0.50 |
1.00 |
0.50 |
0.50 |
0.0870 |
8.70 |
|
BP |
2.00 |
0.50 |
1.00 |
2.00 |
1.00 |
2.00 |
0.1957 |
19.57 |
|
MW |
0.50 |
0.50 |
0.50 |
2.00 |
0.50 |
1.00 |
0.1109 |
11.09 |
[PN: size of population; PD: pressure of population; UP: urban population; EP: elderly population; BP: population of below national poverty line; MW: % of marginal worker]
Table 4: Relative weights of promoting factors
|
Sl. No. |
Theme |
Classes |
Intensity |
Ranks |
Normalized Weights |
Influence (%) |
|
1. |
PN (‘000) |
Upto 1000 |
VL |
1 |
0.1389 |
13.89 |
|
1000 - 2000 |
L |
2 |
||||
|
2000 - 3000 |
ML |
3 |
||||
|
3000 - 4000 |
M |
4 |
||||
|
4000 - 5000 |
MH |
5 |
||||
|
5000 - 6000 |
H |
6 |
||||
|
Above 6000 |
VH |
7 |
||||
|
2. |
PD |
Upto 50 |
VL |
1 |
0.1773 |
17.73 |
|
50 - 100 |
L |
2 |
||||
|
100 - 150 |
ML |
3 |
||||
|
150 - 200 |
M |
4 |
||||
|
200 - 250 |
MH |
5 |
||||
|
250 - 300 |
H |
6 |
||||
|
Above 300 |
VH |
7 |
||||
|
3. |
UP |
Upto 10 |
VL |
1 |
0.2457 |
24.57 |
|
10 - 20 |
L |
2 |
||||
|
20 - 30 |
ML |
3 |
||||
|
30 - 40 |
M |
4 |
||||
|
40 - 50 |
MH |
5 |
||||
|
50 - 60 |
H |
6 |
||||
|
Above 60 |
VH |
7 |
||||
|
4. |
EP |
Upto 2 |
VL |
1 |
0.0870 |
8.70 |
|
2 - 4 |
L |
2 |
||||
|
4 - 6 |
ML |
3 |
||||
|
6 - 8 |
M |
4 |
||||
|
8 - 10 |
MH |
5 |
||||
|
10 - 12 |
H |
6 |
||||
|
Above 12 |
VH |
7 |
||||
|
5. |
BP |
Upto 10 |
G |
1 |
0.1957 |
19.57 |
|
10 - 20 |
AG |
2 |
||||
|
20 - 30 |
F |
3 |
||||
|
30 - 40 |
AF |
4 |
||||
|
40 - 50 |
P |
5 |
||||
|
50 - 60 |
AP |
6 |
||||
|
Above 60 |
B |
7 |
||||
|
6. |
MW |
Upto 2 |
G |
1 |
0.1109 |
11.09 |
|
2 - 4 |
AG |
2 |
||||
|
4 - 6 |
F |
3 |
||||
|
6 - 8 |
AF |
4 |
||||
|
8 - 10 |
P |
5 |
||||
|
10 - 12 |
AP |
6 |
||||
|
Above 12 |
B |
7 |
[VL: very low; L: low; ML: moderately low; M: moderate; MH: moderately high; H: high; VH: very high; G: good; AG: approaching to good; F: fair; AF: approaching to fair; P: poor; AP: approaching to poor; B: bad]
Large population size with high population density was found to promote a high risk of COVID-19 in Assam, followed by Tripura. A moderate risk of promoting the pandemic was found in Mizoram, Manipur, and Nagaland. Sikkim and Meghalaya were found to have low risk, while Arunachal Pradesh has a very low risk of promoting COVID-19 (Fig. 4).
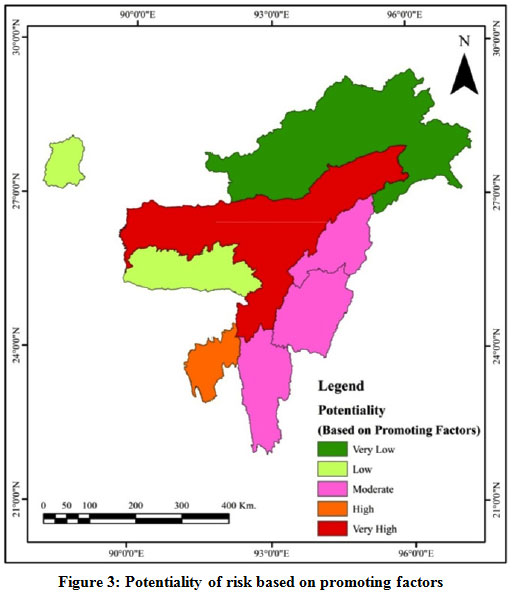 |
Figure 3: Potentiality of risk based on promoting factors Click here to view figure |
Controlling Factors
Among the controlling factors (Annexure-2), the most influencing factors were availability of doctors (24.01%) and available testing laboratories (24.01%) followed by other health workers (14.84), bed available in public health facilities (10.99%), good governance health index (8.08%), number of public health facilities (7.27%) per capita income (6.40%) and good governance composite index (4.40%) as shown in Table 5. The results based on relative weights (Table 6) and overlay analysis (Fig. 6) ranges from 4.72 to 6.31, which was categorized into five classes viz. very high (4.72-5.22), high (5.22-5.61), moderate (5.61-5.86), low (5.86-6.01) and very low (6.01-6.31).
The results show that Assam and Meghalaya have very low potentiality while Tripura has a low potentiality to control the present pandemic situation. A moderate potentiality to control the situation was found in Arunachal Pradesh, and Nagaland and Manipur have high potentiality while Sikkim and Mizoram have a very high potentiality to control COVID-19.
Table 5: Pairwise comparison matrix of controlling factors
|
DN |
HW |
PH |
BD |
GH |
GC |
PC |
TL |
Normalized Weights |
In % |
|
|
DN |
1.00 |
2.00 |
4.00 |
3.00 |
3.00 |
4.00 |
3.00 |
1.00 |
0.2401 |
24.01 |
|
HW |
0.50 |
1.00 |
3.00 |
2.00 |
2.00 |
3.00 |
2.00 |
0.50 |
0.1484 |
14.84 |
|
PH |
0.25 |
0.33 |
1.00 |
0.50 |
1.00 |
2.00 |
2.00 |
0.25 |
0.0727 |
7.27 |
|
BD |
0.33 |
0.50 |
2.00 |
1.00 |
2.00 |
3.00 |
2.00 |
0.33 |
0.1099 |
10.99 |
|
GH |
0.33 |
0.50 |
1.00 |
0.50 |
1.00 |
2.00 |
2.00 |
0.33 |
0.0808 |
8.08 |
|
GC |
0.25 |
0.33 |
0.50 |
0.33 |
0.50 |
1.00 |
0.50 |
0.25 |
0.0440 |
4.40 |
|
PC |
0.33 |
0.50 |
0.50 |
0.50 |
0.50 |
2.00 |
1.00 |
0.33 |
0.0640 |
6.40 |
|
TL |
1.00 |
2.00 |
4.00 |
3.00 |
3.00 |
4.00 |
3.00 |
1.00 |
0.2401 |
24.01 |
[DN: availability of doctors; HW: other health workers; PH: public health facilities; BD: bed available in public health facilities; GH: Good Governance Health Index; GC: Good Governance Composite Index; PC: Per Capita Income; TL: available testing laboratories]
Table 6: Relative weights of controlling factors
|
Sl. No. |
Theme |
Classes |
Intensity |
Ranks |
Normalized Weights |
Influence (%) |
|
1. |
DN |
Upto 30 |
VL |
7 |
0.2401 |
24.01 |
|
30 - 60 |
L |
6 |
||||
|
60 - 90 |
ML |
5 |
||||
|
90 - 120 |
M |
4 |
||||
|
120 - 150 |
MH |
3 |
||||
|
150 - 180 |
H |
2 |
||||
|
Above 180 |
VH |
1 |
||||
|
2. |
HW |
Upto 150 |
VL |
7 |
0.1484 |
14.84 |
|
150 - 300 |
L |
6 |
||||
|
300 - 450 |
ML |
5 |
||||
|
450 - 600 |
M |
4 |
||||
|
600 - 750 |
MH |
3 |
||||
|
750 - 900 |
H |
2 |
||||
|
Above 900 |
VH |
1 |
||||
|
3. |
PH |
Upto 4 |
VL |
7 |
0.0727 |
7.27 |
|
4 - 8 |
L |
6 |
||||
|
8 - 12 |
ML |
5 |
||||
|
12 - 16 |
M |
4 |
||||
|
16 - 20 |
MH |
3 |
||||
|
20 - 24 |
H |
2 |
||||
|
Above 24 |
VH |
1 |
||||
|
4. |
BD |
Upto 60 |
VL |
7 |
0.1099 |
10.99 |
|
60 - 120 |
L |
6 |
||||
|
120 - 180 |
ML |
5 |
||||
|
180 - 240 |
M |
4 |
||||
|
240 - 300 |
MH |
3 |
||||
|
300 - 360 |
H |
2 |
||||
|
Above 360 |
VH |
1 |
||||
|
5. |
GH |
Upto 0.3 |
B |
7 |
0.0808 |
8.08 |
|
0.3 - 0.4 |
AP |
6 |
||||
|
0.4 - 0.5 |
P |
5 |
||||
|
0.5 - 0.6 |
AF |
4 |
||||
|
0.6 - 0.7 |
F |
3 |
||||
|
0.7 - 0.8 |
AG |
2 |
||||
|
Above 0.8 |
G |
1 |
||||
|
6. |
GC |
Upto 3.3 |
B |
7 |
0.0440 |
4.40 |
|
3.3 - 3.6 |
AP |
6 |
||||
|
3.6 - 3.9 |
P |
5 |
||||
|
3.9 - 4.2 |
AF |
4 |
||||
|
4.2 - 4.5 |
F |
3 |
||||
|
4.5 - 4.8 |
AG |
2 |
||||
|
Above 4.8 |
G |
1 |
||||
|
7. |
PC |
Upto 80000 |
VL |
7 |
0.0640 |
6.40 |
|
80000 - 120000 |
L |
6 |
||||
|
120000 - 160000 |
ML |
5 |
||||
|
160000 - 200000 |
M |
4 |
||||
|
200000 - 240000 |
MH |
3 |
||||
|
240000 - 280000 |
H |
2 |
||||
|
Above 280000 |
VH |
1 |
||||
|
8. |
TL |
Upto 1 |
VL |
7 |
0.2401 |
24.01 |
|
1 - 2 |
L |
6 |
||||
|
2 - 3 |
ML |
5 |
||||
|
3 - 4 |
M |
4 |
||||
|
4 - 5 |
MH |
3 |
||||
|
5 - 6 |
H |
2 |
||||
|
Above 6 |
VH |
1 |
[VL: very low; L: low; ML: moderately low; M: moderate; MH: moderately high; H: high; VH: very high; B: bad; AP: approaching to poor; P: poor; AF: approaching to fair; F: fair; AG: approaching to good; G: good]
The results show that Assam and Meghalaya have very low potentiality while Tripura has a low potentiality to control the present pandemic situation. A moderate potentiality to control the situation was found in Arunachal Pradesh, and Nagaland and Manipur have high potentiality while Sikkim and Mizoram have a very high potentiality to control COVID-19.
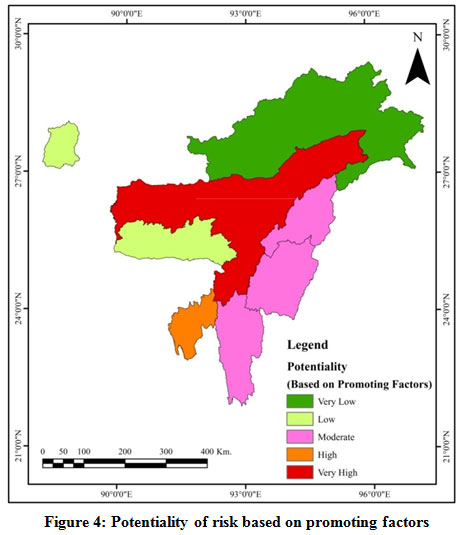 |
Figure 4: Potentiality of controlling the pandemic. Click here to view figure |
A glance at COVID-19 in NEI
Since the first infection of COVID-19 in Manipur on 24th March 2020, it took around 24 days to reach 50 confirmed cases. It took only 18 days to reach 100 confirmed cases on 4th May 2020 then it took just four days to double the figure from 100 to 200 confirmed cases. An unexpected rise in the COVID-19 patients in Tripura and steady infections in Assam has resulted in the number to cross 200 marks24. In Assam, the first COVID-19 case was detected on 31st March 2020 from Karimganj district, which was the 3rd confirmed case in NEI after one case each from Manipur and Mizoram25. At present, most of the reported cases of COVID-19 are from the quarantine centers, and the death rate from COVID-19 is very low (Fig. 7) with only six deaths recorded out of 4,633 confirmed cases as on 11th May 20209. Among the states, Assam has the highest 3,092 confirmed cases of COVID-19 as on 11th June 2020 (Fig. 8). The total number of active cases in Assam was 1,893, followed by Tripura with 655 cases.
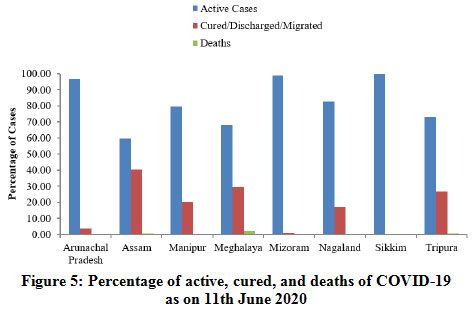 |
Figure 5: Percentage of active, cured, and deaths of COVID-19 as on 11th June 2020 Click here to view figure |
Risk Zonation Mapping
Based on the relative weights of promoting and controlling factors (Table 7), the potential risk zones of COVID-19 generated thereof has been shown in Fig. 9. The result of the map varies from 1.50 to 5.01, which were categorized into five risk zones viz. Very Low (1.50-1.67), Low (1.67-2.04), Moderate (2.04-2.99), High (2.99-3.99) and Very High (3.99-5.01).
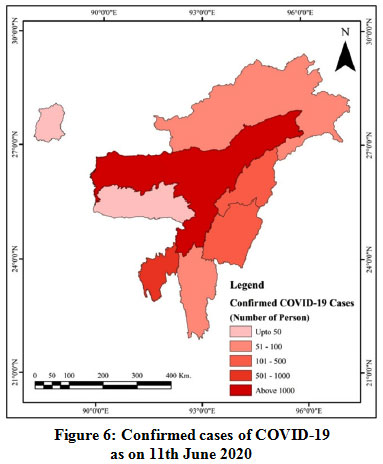 |
Figure 6: Confirmed cases of COVID-19 as on 11th June 2020 Click here to view figure |
Table 7: Relative weights of risk zonation
|
Sl. No. |
Theme |
Classes |
Ranks |
Influence |
|
1. |
Promoting Factor |
VL |
1 |
0.5 (50%) |
|
L |
2 |
|||
|
M |
3 |
|||
|
H |
4 |
|||
|
VH |
5 |
|||
|
2. |
Controlling Factor |
VL |
5 |
0.5 (50%) |
|
L |
4 |
|||
|
M |
3 |
|||
|
H |
2 |
|||
|
VH |
1 |
[VL: very low; L: low; M: moderate; H: high; VH: very high]
Based on factors considered in the study, the predictions revealed that Assam and Tripura would fall in the very high risk zone of COVID-19 and Meghalaya and Nagaland in high risk zone. Manipur is likely to have a moderate risk of COVID-19. Comparatively, Arunachal Pradesh and Mizoram are likely to have low risk, whereas Sikkim has a very low risk of COVID-19. The regional disparities in population characteristics and public health facilities in Assam and Tripura are likely to contribute to COVID-19 cases rapidly. Both the states scored poorly in terms of controlling factors and likely to fail in containing the pandemic in the long run.
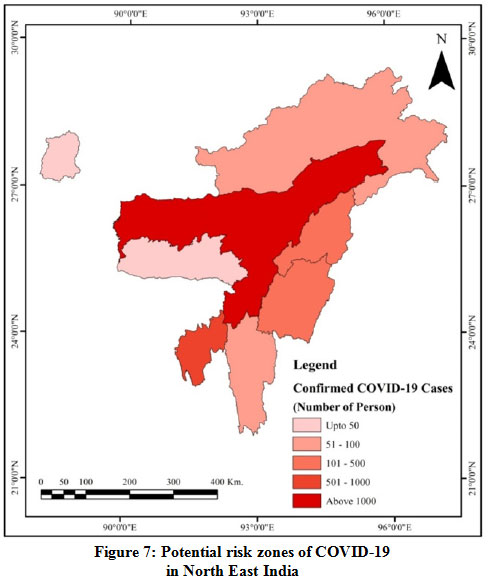 |
Figure 7: Potential risk zones of COVID-19 in North East India |
Overall, Assam and Tripura constitute 49.40% of the total population of NEI. Although the confirmed COVID-19 cases at present are low, the severity of COVID-19 is likely to amplify at a much faster rate in the coming days. A total population of 27.53% fall under high risk zone, 6.92% under moderate risk zone, 12.69% under low risk zone, and 3.45% in a very low risk zone. A general trend of high risks in densely populated states compared to sparsely populated states was found. The results also show a high to very high risk of COVID-19 in the states with significantly less testing laboratory facilities coupled with inadequate public health facilities. Further, the states with a high percentage of below poverty line population and marginal workers may also contribute to the rising cases of the pandemic. Guwahati (the largest urban center of NEI) plays a vital role in increasing cases of COVID-19. At present, the Himalayan hilly states (Arunachal Pradesh, Mizoram, and Sikkim) have reported lesser cases of COVID-19 due to remote location and inaccessibility. These states have the opportunity of more time to organize themselves in fighting against COVID-19 through imposing effective measures and precautions.
Concluding Remarks
The study shows the applicability of AHP and GIS in delineating the risk zones of COVID-19 in North East India. The urban population, population density, population below the national poverty line, population size, the proportion of marginal workers, and the percentage of the elderly population appears to play an essential role in promoting Covid-19 in North East India. While the influence of testing laboratory, availability of doctors, other health workers, bed available in public health facilities, and good governance health index plays an essential role in controlling COVID-19 in the region. Assam and Tripura have a higher risk of promoting COVID-19 transmission in a very short period. On the other hand, Assam, Meghalaya, and Tripura have very weak means to control the severity of COVID-19. Overall, Assam, Tripura, Meghalaya, and Nagaland have a high risk of COVID-19, while Mizoram, Arunachal Pradesh, and Sikkim have a lower risk. Therefore, the respective state governments need to assess their strengths and weaknesses and develop strategic plans to fight against the pandemic. Lastly, frequent testing of COVID-19, immediate quarantine of suspected people, proper social distancing, and regular practice of face mask and hand sanitizer may decelerate the transmission rate of the disease in the absence of a vaccine of COVID-19.
Acknowledgments
The authors acknowledge the Government of India (especially the Central Bureau of Health Intelligence, Ministry of Health & Family Welfare, Central Statistics Office, Ministry of Statistics and Programme Implementation, North Eastern Council Secretariat, Department of Administrative Reforms & Public Grievances, Economic & Statistical Organisation and Indian Council of Medical Research) and the World Health Organization for making available the necessary information required to carry out the study. We also express gratitude to the Department of Geography, Rajiv Gandhi University, Rono Hills, Doimukh for providing infrastructural and laboratory facilities.
Conflict of Interest
There is no conflict of interest in this manuscript.
Funding Sources
Author did not receive any financial assistance from anywhere.
References
- WHO 2020. Coronavirus disease 2019 (COVID-19) Situation Report – 1. January 21 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4 (Accessed on 17th May 2020).
- Boulos M. N. K, Geraghty E. M. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (COVID-19) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int. J. Health Geogr. 2020; 19(1): 8. https://doi.org/10.1186/s12942-020-00202-8
CrossRef - Lipsitch M, Swerdlow D. L, Finelli L. Defining the epidemiology of Covid-19—studies needed. N. Engl. J. Med. 2020; 382(13): 1194-1196.
CrossRef - The Hindu (2020). The failure of the Indian research community to respond to the imminent threat with sufficient alacrity is surprising. https://www.thehindu.com/sci-tech/science/researchers-in-india-must-join-the-fightagainst-covid-19/article31204377.ece (Accessed on 22nd May 2020)
- Prasad R, Perappadan B. S, Shelar J, Koshy J. The Pandemic Notebook: A handy guide from The Hindu on understanding the coronavirus pandemic and staying protected against COVID-19. The Hindu. 2020; https://creatives.thehindu.com/covid_19_ebook.pdf (Accessed on 17th May 2020).
- WHO 2020. Coronavirus disease 2019 (COVID-19) Situation Report – 52. March 12 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200312-sitrep-52-covid-19.pdf?sfvrsn=e2bfc9c0_4 (Accessed on 17th May 2020).
- WHO 2020. Coronavirus disease 2019 (COVID-19) Situation Report – 51. March 11 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 (Accessed on 17th May 2020).
- Deka R. Human Development in Northeast, Sentinel Digital Desk. 24 July 2019; https://www.sentinelassam.com/editorial/human-development-in-northeast (Accessed on 10th June 2019).
- MoHFW 2020. Ministry of Health and Family Welfare, Government of India. https://www.mohfw.gov.in (Accessed on 11th June 2020).
- India TV 2020. Manipur reports first confirmed COVID-19 case. India TV News Desk, Imphal https://www.indiatvnews.com/news/india/manipur-reports-first-confirmed-covid-19-case-600931 (Accessed on 11th May 2019)
- The Hindu 2020. PM Modi announces 21-day lockdown as COVID-19 toll touches 12. https://www.thehindu.com/news/national/pm-announces-21-day-lockdown-as-covid-19-toll-touches-10/article31156691.ece (Accessed on 03rd May 2020).
- National Health Profile 2019. Demographic Indicators. National Health Profile, 2019 14th issue. Central Bureau of Health Intelligence, Directorate of Health Services, Ministry of Health & Family Welfare, New Delhi. http://www.cbhidghs.nic.in/showfile.php?lid=1147 (Accessed on 10th April 2020).
- Census of India 2011. https://censusindia.gov.in/2011census/C-series/C-13.html (Accessed on 15th May 2020).
- National Commission on Population 2019. Population Projections for India and States 2011 – 2036. Report of the Technical Group on Population Projections, Ministry of Health & Family Welfare, New Delhi. https://nhm.gov.in/New_Updates_2018/Report_Population_Projection_2019.pdf (Accessed on 25th April 2020).
- Central Statistics Office 2016. Elderly in India – Programmes and Profile. Ministry of Statistics and Programme Implementation, Government of India, New Delhi. http://mospi.nic.in/sites/default/files/publication_reports/ElderlyinIndia_2016.pdf (Accessed on 25th April 2020).
- National Statistical Office 2020. Sustainable Development Goals, National Indicator Framework, Progress Report, 2020. Ministry of Statistics and Programme Implementation, Government of India, New Delhi. http://www.mospi.gov.in/sites/default/files/publication_reports/SDGProgressReport2020.pdf (Accessed on 25th April 2020).
- North Eastern Council 2015. Basic Statistics of North Eastern Region, 2015. North Eastern Council Secretariat (Evaluation and Monitoring Sector), Shillong, Government of India. http://necouncil.gov.in/sites/default/files/uploadfiles/BasicStatistic2015-min.pdf (Accessed on 15th May 2020).
- Anand S, Fan V. The Health Workforce in India. World Health Organization, Geneva, Switzerland; 2016. pp. 1-98. Human Resources for Health Observer Series No. 16. https://www.who.int/hrh/resources/16058health_workforce_India.pdf (Accessed on 10th April 2019).
- Press Information Bureau 2018. Hospitals in the Country. Government of India, New Delhi. https://pib.gov.in/PressReleasePage.aspx?PRID=1539877 (Accessed on 30th April 2020).
- Centre for Good Governance 2019. Good Governance Index. Department of Administrative Reforms & Public Grievances, Ministry of Personnel, Public Grievances and Pensions, New Delhi. http://pibarchive.nic.in/newsite/erelease.aspx?relid=196119 (Accessed on 25th April 2020).
- Economic & Statistical Organization, Punjab 2020. State wise data on Per Capita Income. Government of Punjab, Chandigarh. https://www.esopb.gov.in/static/PDF/GSDP/Statewise-Data/statewisedata.pdf (Accessed on 25th April 2020).
- ICMR 2020. Total Operational (initiated independent testing) Laboratories reporting to ICMR, Indian Council of Medical Research Department of Health Research, Ministry of Health and Family Welfare, Government of India. https://www.icmr.gov.in/pdf/covid/labs/COVID_Testing_Labs_11062020.pdf (Accessed on 11th June 2020).
- Saaty T. L. 1980. The analytic hierarchy process. McGraw-Hill, New York.
CrossRef - Hindustan Times 2020. Covid-19 cases in North-East double from 100 to past 200 in just 4 days. https://www.hindustantimes.com/india-news/covid-19-cases-in-north-east-double-from-100-to-past-200-in-just-4-days/story-iQliVrMGLlVgISGdG3LjaL.html (Accessed on 11th June 2020).
- The Assam Tribune 2020. First COVID-19 Case in State. http://www.assamtribune.com/scripts/at.asp?id=apr0120/Page1 (Accessed on 25th April 2020).






